What’s in a number? … For the vanguards of revenue cycle management — treasurers, government reimbursement administrators, cost accounting directors, controllers, chief financial officers, and billing and collections managers — a number can have special meaning if it happens to be a key performance indicator (KPI) in the healthcare industry.
These medical industry professionals rely on KPIs for a variety of financial functions including auditing, budgeting, building analytical models, maintaining cash flow, cost reporting, monthly and year-end statements, monitoring accounting systems and revenue cycle strategies.
Tracking numbers in relation to patient care may seem cold and calculated, but maintaining an efficient revenue cycle is the “necessary evil” that enables hospitals and other institutions to remain profitable and  continue providing personalized healthcare to a variety of age groups.
continue providing personalized healthcare to a variety of age groups.
With knowledgeable administrators maintaining cash flow at the back end, physicians and support staff are able to focus on patient care versus filing time-consuming forms and reports.
The topic in part two of this series is the Account Resolution stage, an important cluster of KPIs indicating the effectiveness and status of mid-cycle compensation channels. The HFMA Map Keys page provided sources for some of this information.
Account Resolution
Monitoring and maintaining financial stability is a daily activity indicating an institution’s ability to provide reliable healthcare to patients in the community. A review of Accounts Receivable Aging Reports, including  the gross amount existing in buckets categorized by the number of days they remain unpaid, is a good place to start.
the gross amount existing in buckets categorized by the number of days they remain unpaid, is a good place to start.
Accounts Receivable (A/R) is generally grouped into aging buckets based on 30-day increments of elapsed time from the day of service or discharge: pending insurance payments, 0 – 30 days, 31 – 60 days, 61 – 90 days, 91 – 120 days, 121 – 150 days, and greater than 150 days.
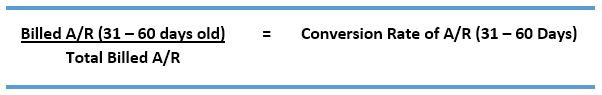
Next, examine the aged accounts receivable as a percentage of the total invoiced accounts receivable to reveal the effectiveness of collecting A/R. This KPI is determined by formulating simple proportions for the aging categories mentioned above. (The grand total of all KPIs should equal 100 percent.)
For the 31 – 60 days category, for example, the KPI is calculated by dividing the invoiced amount in that category by the grand total of billed receivables:
 Reviewing all aging groups is necessary, but two categories resonate “loudly” in revenue cycle management.
Reviewing all aging groups is necessary, but two categories resonate “loudly” in revenue cycle management.
Percentage of Accounts Receivable Over 90 days
Under ideal conditions, healthcare institutions should pursue accounts receivable immediately after 30 days instead of waiting until 60 or 90 days. Nevertheless, the KPI for unpaid balances over 90 days should be 17 – 20 percent excluding active billed credit balance accounts, discharged not final billed (DNFB) accounts, in-house accounts, or in-house interim-billed accounts.
 A high ratio in this area indicates failure to collect from problematic claims or certain categories of payers, delays in submitting prompt claims, missing or incorrect data on claims, or gaps in care documentation.
A high ratio in this area indicates failure to collect from problematic claims or certain categories of payers, delays in submitting prompt claims, missing or incorrect data on claims, or gaps in care documentation.
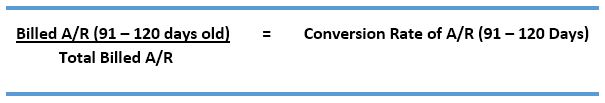
Acknowledging the negative consequences of A/R in the over 90-day category, having it greater than 120 days is considerably worse given the low expectations of collecting older debt. A KPI of less than 12 percent is recommended in this category.
Charity Care
Healthcare institutions often provide uncompensated care to patients who are unable to pay because of economic factors such as low income, unemployment or death of a family bread winner.
Charity care status is usually determined prior to treatment or admission, but it is sometimes granted retroactively including emergency situations.
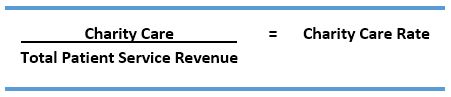 A rate of 2 percent or less is a good ratio for most hospitals.
A rate of 2 percent or less is a good ratio for most hospitals.

Bad Debt
The Bad Debt KPI is a catch-all for uncollected debt by institutions: controllable sources such as faulty claims follow-up and uncontrollable factors such as insurance companies denying claims retroactively or patients who are unwilling or unable to pay.
For patients with insurance, unpaid deductibles and coinsurance are considered bad debt if patients cannot or will not pay the balance. For uninsured patients, bad debt may pertain to all or just a portion of unpaid services.
 Gross Collections
Gross Collections
Gross Collection ratios of 95 percent or more are desirable for healthcare institutions. Those with more than 5 percent in unpaid claims need to examine the revenue management cycle and search for clues leading to the anomalies including the claim filed with specific insurance providers, flaws in the claims or billing processes, or difficulties with certain demographics or regions.
Closing Words About Revenue Cycle Management
Disproportionate ratios in these last three areas of uncompensated care — charity care, bad debt and low collection rates — could spell disaster for healthcare institutions.
 A KPI is just a number, but for institutions experiencing poor performance, the immediate goal is to identify the problem, determine the root and reach of the problem, and finally, look for solutions to fixing the problem.
A KPI is just a number, but for institutions experiencing poor performance, the immediate goal is to identify the problem, determine the root and reach of the problem, and finally, look for solutions to fixing the problem.
Understanding the dynamics of KPIs in revenue cycle management is an important component of monitoring and improving revenue cycle performance in the healthcare industry. Furthermore, applying industry standards enables institutions to compare their metrics against other organizations and gain insight into patient trends. More importantly, though, maintaining ratios within the acceptable standards creates the sound financial basis that satisfies stakeholder interests and provides a level of service to the community that is both uncompromised and sustainable.
The third and final part of this series is an overview of important metrics in revenue cycle management such as Days in Accounts Receivable, Net Collection Rate and the Cost to Collect. (Part one covered the early stages of Patient Access and Claims while part three covered the Financial Management KPIs pertaining to late-stage revenue cycle management).
Finally, healthcare organizations in search of external debt collection agencies may contact Optio Solutions to learn about its best-in-class foundation of compliance, certification, data security and technology and individualized strategies offering a favorable return on investment and brand protection.